MANILA -- The Philippine Health Insurance Corporation (PhilHealth) on Saturday clarified that the alleged overpayments made in its claims amounting to PHP154 billion in the past six years are efficiency gains, a feature in the case rates payment system that the agency is implementing.
In a statement, the PhilHealth the efficiency gains is used to "effectively impose the No Balance Billing (NBB) policy for sponsored program members admitted in ward or ward-type accommodations in government health care institutions" and that it is "currently paying its health care providers using case rates, a fixed amount that covers both hospital and professional charges".
The PhilHealth issued the statement in response to a news report on Friday, saying PhilHealth had "increasing payments for pneumonia from 2010 to 2018, reaching “epidemic proportions” when there was no outbreak of pneumonia declared by the Department of Health (DOH)".
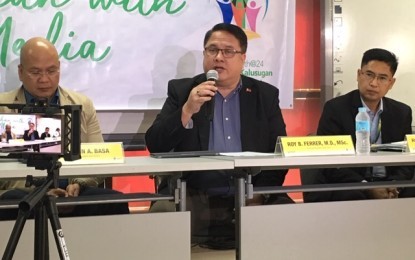
PhilHealth acting president and chief executive officer Roy Ferrer said the DOH's data are based on public health units or facilities, while PhilHealth’s claims statistics are based on actual payments of claims made to its health care providers, so, both figures cannot be compared.
“The case rates are so designed such that facilities can 'win some and lose some.' If these facilities are efficient in patient management, they would be able to save on costs and gain from the reimbursements process to offset those losses when they fail to contain costs in other patients. This is also applicable to public hospitals which bear the rest of the costs under the NBB policy,” he said.
Referring to what the article said the PhilHealth lost some PHP51.2 billion out of the PHP154 billion due to fraud between 2013 and 2018, Ferrer said "there is no health insurance system in the entire world that is fraud-free and the 10 percent standard is applied when no efforts are exerted by the insurer to correct leakages."
Ferrer disclosed that 1,251 counts of pneumonia cases from 162 providers are under probe at the agency's prosecution department, adding that the PhilHealth has already decided on 34 cases against 14 facilities and professionals within the first quarter of 2019.
"PhilHealth is also currently hearing 4,419 cases more made up of recently received cases, carry-over cases and reopened cases for further proceedings. As of April this year, PhilHealth also reported that it has already completed 1,432 investigations and is currently investigating close to 9,000 more reports of fraudulent activities. It was noted that the highest number of cases are coming from regions 4A,10, and 11," he added.
Ferrer reiterated PhilHealth's competence in handling funds entrusted to it "which is proven by its profitability as its net income amounted to PHP11.6 billion at the end of 2018".
"The PHP257 billion Universal Health Care fund includes those allocated for DOH for its service delivery, governance and regulation functions – so the fund is not entirely for PhilHealth alone," he said.
Ferrer said the corporation welcomes the "citizen’s vigilance against those who commit fraud, from inside the walls of PhilHealth and from the outside".
“We can now move forward with our resolute anti-fraud campaign with an awakened citizenry squarely behind us. (I am) issuing a stern warning to those who choose to be our adversary and to be enemies of the state - their deception, stealing and lying will be exposed. The truth will prevail,” he added. (PNA)
