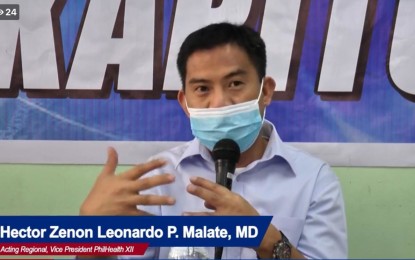
Dr. Hector Zenon Leonardo Malate, acting regional vice president of the Philippine Health Insurance Corporation-Region 12 (Photo screengrabbed during virtual press conference)
GENERAL SANTOS CITY – The Philippine Health Insurance Corporation (PhilHealth) in Region 12 (Soccsksargen) has raised an alert over the proliferation of “fraudulent” wellness programs that prompt residents to undergo unnecessary confinement in hospitals to collect health insurance claims.
Dr. Hector Zenon Leonardo Malate, PhilHealth-12 acting regional vice president, said in an advisory on Monday the questionable activities were reportedly being conducted in parts of the region by several hospitals.
Citing reports received by their office, he said the involved hospitals would hold free medical consultations and make it appear that a PhilHealth member or dependent has an illness or condition that requires hospitalization.
He urged residents, especially their members, to shun from such “solicitation scheme or fraudulent activity.”
“PhilHealth has no wellness program. Members can only avail of their benefits if they are truly ill and require (hospital) confinement,” Malate said.
He advised their members to carefully read any document provided by hospitals or related institutions before signing them.
Malate said they should not sign blank documents, especially those that contain wrong information or declaring that they were hospitalized even if it did not happen.
He said any member who will be involved in such kind of activity or connive with any hospital may face various sanctions, including the recall of their PhilHealth benefits.
This is provided for in Section 38.10, Rule X of the penal provisions of Republic Act 11223 or the Universal Health Care Law, he said.
Aside from this, Malate said the unnecessary or wrongful use of benefits could lead to the full use or saturation of the 45-day benefit allowance of PhilHealth members and their dependents.
“This could result in the non-availment of their benefits by the time that they would need them,” he said.
As of December, PhilHealth-12 already investigated at least 25 hospitals and nine doctors in the region over alleged fraudulent practices and health insurance claims.
Malate said their legal unit conducted fact-finding investigations in various activities based on endorsements from their benefits and administration division.
Most of the violations were for “misrepresentation, (claiming for) non-admitted patients, extending the period of confinement and multiple filing of claims,” he said. (PNA)
